Introduction
While overall survival has improved, patients with high-risk multiple myeloma (MM) have poor outcomes. Fluorescent in situ hybridisation (FISH) is widely used to identify high-risk genomic features at diagnosis, but a significant minority of patients classified with standard-risk disease progress rapidly and in retrospect may have warranted more intense frontline therapy. Recently, we implemented the Myeloma Genome Project Panel (MGPP) into clinical workflows - a myeloma-specific targeted sequencing panel capturing 228 genes, 6 translocation regions and 56 copy number abnormalities (CNAs) in a single assay [PMID: 35522533]. Given that MGPP captures many prognostic regions beyond the limited number assessed by FISH, there is potential to better identify high-risk patients. However, the utility of MGPP in supporting clinical risk designation and therapy choice when compared with FISH in newly diagnosed MM is unknown.
Methods
A prospective cohort study was conducted to compare the impact of MGPP vs. FISH on baseline risk stratification and treatment intention, in 55 unselected newly diagnosed MM patients. For MGPP, libraries were generated from 100ng DNA from bone marrow (BM) derived CD138 + MM cells and matched germline peripheral blood (Roche KAPA HyperCap Target Enrichment/Hyperplus kit). Reads were aligned to hg38, and somatic mutations, CNAs and translocations called with a custom pipeline. ISO-accredited FISH analysis was performed in NHS laboratories. In a multicentre multidisciplinary team (MDT) meeting, four blinded haematologists independently reviewed each clinical case presented twice with either FISH or MGPP, in a random order. Clinicians designated risk status and treatment intentions using a structured proforma. Therapeutically actionable variants could be selected as per the MyDRUG trial [ClinicalTrials.gov: NCT03732703]. A consensus MDT outcome for high-risk or more intensive therapy required at least 3 out of 4 concordant decisions.
Results
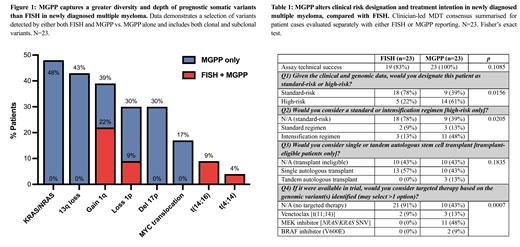
Data is presented here for 23 of 55 patients. The mean age was 68.9 years, 57% were transplant eligible, with R-ISS-1 (35%), R-ISS-2 (26%) and R-ISS-3 (39%). Firstly, MGPP had greater technical success than FISH, reporting successfully in 100% vs. 83% cases from the same diagnostic BM samples respectively (n=4 assay failures with FISH). Secondly, MGPP reported more genomic features than FISH, detecting 231 vs. 18 somatic variants at 127 vs. 7 regions, respectively. Thirdly, MGPP captured equivalent loci at greater resolution, detecting subclonal CNAs missed by FISH (Figure 1). In a head-to-head comparison with FISH, these additional genomic insights from MGPP influenced clinical treatment decisions. A clinician-led MDT reclassified 9 (39%) patients designated as standard-risk by FISH to high-risk status when presented with MGPP (Table 1). Reclassified patients were enriched for prognostically significant MYC translocations (17%) and subclonal 17p loss (22%), 1p loss (17%) and 1q gain (13%) CNAs that were missed by FISH. Altered risk designation influenced frontline treatment intention; clinicians opted for intensification of induction therapy in 13% (FISH) vs. 48% (MGPP) high-risk patients, and considered tandem autologous transplant as an option in 0% (FISH) vs. 23% (MGPP) transplant-eligible patients. FISH identified a therapeutically actionable variant in 3 (13%) patients [venetoclax, n=3]. MGPP identified 13 (57%) additional patients with opportunity for targeted therapy [MEK inhibitor, n=11; BRAF V600E inhibitor, n=2], which the MDT considered as a treatment option in all cases if available in trial. The full dataset and analysis will be presented at time of the conference.
Conclusions
We demonstrate that MGPP impacts clinical risk designation and treatment intention in newly diagnosed MM. MGPP had greater technical assay success than FISH and captured a greater range and depth of somatic variants. Importantly, these additional insights led a clinical MDT to reclassify 39% patients as high-risk, consider intensification regimen in 39% cases and potential for actionable targeted therapy in 57% patients. Our results support MGPP as a robust alternative to FISH in supporting risk-adapted treatment decisions. We will implement MGPP in additional large prospective cohorts over the next year, to better understand its prognostic utility and feasibility in routine clinical workflows.
Disclosures
Ramasamy:Pfizer, GSK: Membership on an entity's Board of Directors or advisory committees; AbbVie, Adaptive Biotechnologies, Amgen, Celgene (BMS), GSK, Janssen, Karyopharm, Oncopeptides, Pfizer, Sanofi, Takeda, Recordati pharma, Menarini Stemline: Speakers Bureau; AbbVie, Adaptive Biotechnologies, Amgen, Celgene (BMS), GSK, Janssen, Karyopharm, Oncopeptides, Pfizer, Sanofi, Takeda Recordati pharma, Menarini Stemline: Honoraria; Amgen, Celgene (BMS), GSK, Janssen, Takeda: Research Funding. Thakurta:Antenegene, Bristol Myers Squibb: Consultancy, Current Employment, Current equity holder in publicly-traded company, Current holder of stock options in a privately-held company, Honoraria, Research Funding. Gooding:Bristol Myers Squibb: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal